Does Acupuncture Work for Pain?
A review of modern acupuncture evidence and myths, focused on treatment of back pain & other common chronic pains
In early 2009, the British Medical Journal published a new analysis of acupuncture for pain … with discouraging results.1 Again! Not the first time, not the last. More dramatically, the journal Pain did it again — one of the top ten journals for pain and injury science. In early 2011, Pain published a thorough and rather harsh scientific smack down of acupuncture, concluding that there is “little truly convincing evidence that acupuncture is effective in reducing pain,”2 or anything else.3 Acupuncture was officially scorned in the UK’s 2016 NICE guidelines for back pain, with the recommendation “do not offer.”45
Even many expert acupuncture proponents have admitted that it doesn’t work, but they cleverly and weirdly spin this as good news.67 For instance, the infamous case of the 2010 New England Journal of Medicine paper: pro-acupuncture authors clearly acknowledged that “sham acupuncture was as effective as real acupuncture” — results that would be unanimously seen as a failure in any drug trial — and yet they endorsed it anyway.8 In 2009, back pain experts Cherkin and Deyo did much the same, reporting results that were quite disappointing … but they bent over backwards to make it sound like good news anyway.9 And there is the infamous case of the Vickers meta-analysis in 2012:10 widely touted as “positive,” Dr. Edzard Ernst described it as “the most compelling evidence yet to demonstrate the ineffectiveness of acupuncture for chronic pain.” A 2017 update changed nothing.11
The acupuncture debate has degenerated into highly polarized interpretations of the same evidence, rather than the publication of useful new evidence. The British Medical Journal stirred the acupuncture pot with dubious motives: in early 2018, they published a debate between Dr. Ernst and an acupuncture booster, which a critic described as, “Just more manufactured doubt from quacks (as used by tobacco industry). Why does BMJ do this so often?”12 Because it gets attention!
And then yet another respected journal! Also in early 2018, PLoS ONE published “one of the worst studies I have ever seen.”13 PLoS ONE seems to be noticing the criticisms, and there may well be a retraction, but meanwhile this “positive” review is being cheerfully cited by acupuncture proponents as if it matters … but it’s just junk.
Meanwhile, many other sources have declared acupuncture ineffective without any attempt to spin it: a major report on treatments for knee osteoarthritis — one of the most common pain problems, and as likely a target for acupuncture as any — declared it to be useless.14 But the one source to rule them all is the taxpayer boondoggle NCCIH, a huge organization funded by American taxpayers to research alternative medicine. They continue to research acupuncture “even though many of its studies have found that acupuncture … works no better than a sham treatment at easing symptoms like pain and fatigue.”15 If these guys won’t say that acupuncture works …
Acupuncture for pain has enjoyed a strong reputation for decades
All of this evidence is in stark contrast to what most people believe about acupuncture. People actually think science supports acupuncture, because of headlines about junk science (like the PLoS ONE paper just mentioned).
But regular people know nothing about what makes a study good or bad … and that includes most healthcare professionals. Doctors are not scientists! And so they think acupuncture is “evidence-based” with no clue just how fatally flawed most acupuncture research actually is.
Acupuncture is not supported by any good research, which is clear to people who actually read the fine print.
And that’s not a surprise, because we’re talking about a healing system that rests on a belief in auras: an alleged “energy” in and around the body that no one can actually detect.16 Or — if not an energy system — some biological version of them that remains as elusive as physical evidence of ghosts, UFOs, or bigfoot.
Somehow, acupuncture has managed to become the poster child of alternative medicine. Almost everyone seems to believe that there “must be something to it.” The term “medical acupuncture” is now ubiquitous, oxymoronic but successful propaganda that makes acupuncture seem more medically legitimate simply by calling it “medical.” Until the last few years, even many hardened skeptics and critics gave it a bit of a pass.17 But beliefs about acupuncture are much more specific than that: health care consumers and professionals particularly tend to believe that acupuncture is “good for pain.”
When North Americans think of using acupuncture for pain relief, they often visualize an almost magical anaesthetic effect. This mental image comes to us direct from the year 1972, when journalist James Reston wrote about his appendectomy during American President Nixon’s trip to China — he was apparently “anaesthetized” with acupuncture needles. Now that’s a dramatic effect!
Mostly because of that old bullshit story — details below — most Westerners still believe that acupuncture is good for pain, if not downright amazing for pain. And, throughout the 1970s, 80s, and 90s scientific research — of questionable quality — seemed to back that up. Even today, plenty of junky acupuncture studies are still constantly published, mostly in only the worst journals, of course, but occasionally even in good ones, like the PLoS ONE example just mentioned, among others.18 Certain countries — Russia, China, we’re looking at you — have produced almost literally nothing but positive acupuncture trial results!19 Funny that.
Garbage in, garbage out: the legacy of all that sloppy, biased research is that we still get research reviews with supposedly happy endings.20 To zoom in on just one, in 2005, the Annals of Internal Medicine looked at all the mostly poor quality evidence that had been produced up to that time and concluded, “Acupuncture effectively relieves chronic low back pain.”21 (And yet, importantly, they also had to admit that, “No evidence suggests that acupuncture is more effective than other active therapies.” Which don’t work very well. Because low back pain is notoriously difficult to treat. More on this below.) There were certainly good reasons for skepticism by then, but it was still all too easy to look at the available research and feel good about acupuncture — especially if you stuck to the Chinese research!
One of the first really meticulous, rigorous modern acupuncture studies finally arrived in 2007, with evidence that acupuncture could outperform some conventional therapies. Sounds good for acupuncture, doesn’t it? Unfortunately, there was a catch …
Real acupuncture versus fake acupuncture: the only contest that matters
The general problem with most acupuncture research, especially the older stuff, is that it had never been well “controlled.” That’s not a minor problem — “controlling” research by comparing a therapy or medicine to a persuasive fake is extremely important. The methodical Germans made note of this, writing that acupuncture has “never been directly compared” with a placebo or with conventional therapy. So they did it.
The results were published in 2007 in Archives of Internal Medicine. It was literally the first ever well-controlled study of acupuncture for back pain. Exciting! This was a big study (good sample size), and well designed. Looks to me like they really put all past research to shame: a “randomized, multicenter, blinded, parallel-group trial.” Phew. That’s all good. And the results are fascinating! There were two clear findings:
- Both acupuncture and sham acupuncture were better than conventional physical drugs, physical therapy, and exercise.
- Acupuncture was no better than sham (fake) acupuncture.
Yes, you read that correctly: acupuncture was no better than a sham (no surprise, totally consistent with other research)… but both acupuncture and the sham were better than conventional therapy. Ouch! Not good news for physical therapists! Or acupuncturists! Sort of? Acupuncture cannot be efficacious if it’s no better than fake acupuncture, so how can they both do better than drugs, physio, and exercise? There’s an apparent contradiction there.
It was a big, weird deal. It was both a significant and strange package of good and bad news for everyone concerned.
The expectation of positive outcome — simple optimism — is a major factor in healing from back pain, probably the greatest. People who believe that they are going to get better, get better.22 And people who receive acupuncture — the real thing or a clever imitation — simply feel better cared for … while conventional therapies simply fail to reassure.
Patients are cynical about conventional therapies, and with good reason. Believe me! I know — I saw it for many years in my work as a massage therapist. That cynism is why alternative health care professionals have busy practices. And it’s justified. Conventional therapies for low back pain are incredibly underwhelming. In fact, they’re so underwhelming that beating them by a little bit is nothing for acupuncture to brag about. All it really means is that acupuncture makes patients feel more cared for and hopeful than conventional therapies do.
This evidence should make patients cynical about acupuncture, too! The authors of the study wrote that the lack of difference between acupuncture groups “forces us to question the underlying action mechanism of acupuncture and to ask whether the emphasis placed on ... traditional Chinese acupuncture points may be superfluous.” Yes, rather!
A fine example of acupuncture research that seems well-designed and positive … but is still bizarrely flawed
Researchers tested acupuncture for chronic shoulder pain on 424 patients.23 One group of patients received Chinese acupuncture in the shoulder, another group received sham acupuncture, and a third group received convential but conservative orthopaedic treatment. Everyone received 15 treatments over a 6-week period. Looking good so far.
The results seemed significant and positive, and the conclusion was glowing.
But wait a moment, what’s this … ? The sham acupuncture was in the leg? For a shoulder pain study?
A sham has to be convincing to bother comparing it to a treatment, and the sham used in this study was not convincing, as the needles were placed in the leg. Patients might not know much about acupuncture, but they certainly would know that sticking needles in a leg probably isn’t a treatment for their shoulder! D’oh. The result is that patients could easily get a huge placebo effect from the “real” treatment, and none at all from the sham.
This absurd paper is dissected in more detail in an excellent article by Neil O’Connell.24
Even when acupuncture research “looks good on paper,” it’s always fatally flawed one way or another. The predictability of it is almost comedic. There are many other examples.25
It has only gotten steadily worse for acupuncture
Haake et al.’s 2007 study was one of many better quality experiments that have now been done. Good modern scientific studies of acupuncture now effectively compare real acupuncture to fake or sham acupuncture, using various tactics,2627 and their results have now been replicated in high impact journals.28
What all this newer research shows, time and again, is that both real acupuncture and fake acupuncture perform equally well. (In fact, sometimes fake acupuncture works better!) That is, they both “work”29 as well as a placebo, neither of them routinely work any miracles, and they have the same effect regardless of whether or not the needles are being used according to the principles of traditional Chinese medicine (TCM).
In general, the higher the quality of the evidence, the more discouraging the results have been for acupuncture. This is a classic pattern to look for when you’re trying to evaluate research. Where is most of the good news coming from? What do the larger, better, newer studies show? Compare and contrast!
Phantom acupuncture: qi and meridians in a rubber hand?
One of the most acupuncture-damning experiments ever conducted was the one that showed that acupuncture can “work” even when the needles are stuck into a rubber hand.30
Subjects had their brains scanned while acupuncture was performed on a “phantom limb,” by tricking the brain into perceiving a rubber hand as if it was real.31 In this scenario, the needling cannot possibly be the cause of a biological response, because rubber hands do not have cells or nerves. And even if people have qi flowing in meridians, clearly rubber hands do not. And so this experiment neatly eliminates two of the major common explanations for how acupuncture might work (as measured by brain scans, anyway).
The results identified the same kind of perceptions and brain activity that previous studies have found with needling of genuine limbs. This (strongly) suggests that the explanation for any perceived benefit of acupuncture is psychological: the brain can obviously respond to the idea of needling. Real needling not required to elicit the same response that has been touted as a specific therapeutic effect. If true, belief is the active ingredient in acupuncture, not the manipulation of qi. This result is perfectly consistent with the skeptical position on acupuncture. Dr. Steve Novella has reported in more detail on this study: see “Phantom Acupuncture.”
Not so ancient after all: acupuncture’s myths
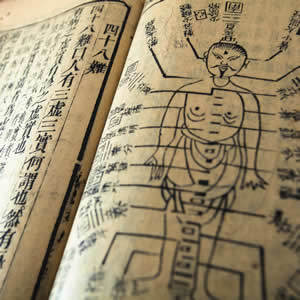
Clinical evidence isn’t the only angle on this topic. Research and scholarship about acupuncture has also produced a constant parade of smart debunkery and historical facts and cultural context that is really quite embarrassing to the Legend of Acupuncture, showing that it has all the characteristics of modern faddism … not ancient Chinese wisdom.
Indeed, even in China, acupuncture’s key concepts have a dubious history and provenance. For instance, Ben Kavoussi, a doctor and acupuncturist himself by training (and therefore an unusually credible critic) has explained how the supposedly “ancient” and mystical meridians of acupuncture are actually based on quite modern and arbitrary interpretations.32
Before that, for most of history, “acupuncture” existed primarily as a form of bloodletting — much like the prescientific medieval European practice — or much worse.333435 So, not so ancient after all.
“The smell could almost be heard.” That image refers to a child’s rotting leg — rotting because of the incompetence of traditional Chinese medicine, as described in The Reality of Ancient Wisdom. This article is essential, morbidly fascinating reading. I didn’t think I could get any more cynical about ancient folk medicine. I was wrong! Dr. Hall packages up a few excerpts from an old book by a physician working in China in the late 19th Century. His matter-of-fact reports of the actual medical habits of the Chinese at that time are chilling, and a harsh reminder that traditional Chinese medicine was not wise and profound, but rather cringe-inducingly horrible, just as brutal and bizarre as any pre-scientific European “medicine.” In particular, the stories concerning acupuncture expose a mess of superstitious and vicious excess. Bloodletting was the tip of the iceberg. Little wisdom is possible in a state of profound ignorance.36 TCM is not wise: it’s a patchwork of superstition, habit, and guess work.37
Then there’s the myth of acupuncture’s popularity. Even its alleged popularity and widespread use in China is quite trumped up — it is, for instance, not really used for anaesthesia. The anaesthia and popularity myths will be described more below.
Such historical perspectives are extremely useful in understanding how naively over-rated acupuncture has become in the world today. Always remember: foolishness is more ancient than wisdom.
“I put the needles in me instead of in you.”
But is acupuncture actually even popular?
Probably not nearly as popular as acupuncturists want us to think it is. Brennen McKenzie for ScienceBasedMedicine.org:38
I don’t believe the quality of the data generally allow very confident statements about the popularity of acupuncture. However, proponents of acupuncture often make such statements, trying to convey the impression that their approaches are growing rapidly in popularity and only perverse, closed-minded curmudgeons still resist them. The little evidence we have certainly does not support such claims.
There’s no question that acupuncture is somewhat popular: it’s certainly on the public’s radar as an option, something that might be “worth a shot.” However, it is still an option that mostly only desperate pain patients try, and no way is it even nipping at the heels of mainstream medicine in terms of “market share”; it remains a trivial, marginalized player in health care.39 It is not even remotely winning over every patient. Only quite rarely do I hear from a reader or a patient who “swears by” acupuncture, and of course the most emphatic testimonials invariably suffer from obvious flaws, such as recovery that could well have been powered by placebo, a concurrent treatment, or coincidence with natural healing.
Far more commonly, the reports are tepid and uncertain — “I think it might have made a difference” — or frankly negative — “Didn’t do a thing. Waste of money.” Hardly the stuff of serious popularity there.
If acupuncture is popular, it certainly isn’t saving the world from pain. All kinds of chronic pain problems continue to plague North Americans — quite possibly in record numbers, especially low back pain.40 After working for more than decade with chronic pain patients of all kinds, I have yet to see anyone “cured” by acupuncture, even though large numbers of my clients and readers have certainly tried it.41
What about the anesthesia thing? Another myth …
James Reston and the “acupuncture anaesthesia” myth
So … what really happened to James Reston? Did he actually have surgery without anaesthetic?
He did not! This isn’t even controversial: the popular version of the story is just factually incorrect. And yet it’s almost single-handedly responsible for the popularity of acupuncture outside China.
By his own account, Reston was chemically anaesthetized in a thoroughly medical manner, an epidural — “a normal injection of Xylocain and Benzocain, which anesthetized the middle of my body … and then pumped the area anesthetic by needle into my back.” And, by his own account, Reston received no acupuncture of any kind until 24 hours later, and even that was for “considerable discomfort” — not the severe pain assumed by virtually all re-tellings of the story.
These details are described in a thorough series for ScienceBasedMedicine.org.42 Dr. Kimball Atwood presents a strong case that the “acupuncture anesthesia” promoted from about 1958 through the mid-1970s by the People’s Republic of China — and becoming a powerful myth in North America and Europe — was essentially faked. Like Reston, most patients who underwent acupuncture for surgery were given also sedatives, narcotics, and local anesthetics. Statistics about the use and effectiveness of “acupuncture anesthesia” were grossly exaggerated. During the Cultural Revolution, patients were under extreme pressure to please their physicians and any authority figures — such as a Party representative proudly, conspicuously presiding over the procedure! — which meant they were rather unlikely to complain, even if it meant enduring a lot of pain.
Although it’s true that people can withstand painful procedures without anesthesia to a greater extent than is generally acknowledged in this era of safe anesthesia, the history of acupuncture “anesthesia” in the Peoples’ Republic of China is mainly one of state-sponsored torture.
Dr. Kimball Atwood
In the late 1970s, when criticism became safe, knowledgeable doctors began speaking out publicly about the fakery, and use of and respect for Traditional Chinese Medicine has been declining in China since that time. Significantly, there is no longer any acupuncture anesthesia or analgesia — at least not to an extent that is either humane or clinically useful for surgery.
Acupuncture treatments, as sold in most places, are used to try to treat specific health conditions and chronic pain. Even if that worked, a true I-can’t-feel-anything anaesthetic effect would be a totally different animal (and a much bigger one). Using acupuncture for true anaesthesia actually is almost as impossible and absurd as it sounds. You don’t want to try it, any more than you want to try getting a tooth pulled after a good belt of whisky.
It’s actually not all that unusual for human beings to endure awful things without any kind of anaesthetic. My father, a Vietnam veteran who has both witnessed and experienced extreme traumas, demonstrates this himself occasionally by submitting to dental drilling without freezing — “I hate the freezing so much, I’d rather just deal with the pain and get it over with.” There are numerous social and personal factors that can lead to high pain tolerance … and it can be completely situational. Ask any nurse or doctor: people are full of surprises, and often hurt much less (or much more) than you might expect.
In her book, Women Aren’t Supposed to Fly: The memoirs of a female flight surgeon, Dr. Harriet Hall tells the story of a man who got a vasectomy without anesthesia because he was mistakenly injected with saline solution rather than lidocaine. She also tells the story of a woman whose severe headaches went away after being injected with saline. The latter swore that only Demerol worked for her, but she had been conditioned to feel relief when she got a shot. Likewise, the vasectomy victim didn’t feel excruciating pain because he also was conditioned to get pain relief from certain injections.
The Skeptic’s Dictionary, “Acupuncture”
So, while it might seem spooky that anyone has used acupuncture as an “anaesthetic,” it’s actually just not nearly as interesting a phenomenon as it might seem to be at first. Madsen et al. interpret this kind of pseudo-anaesthesia effects as a dramatic example of a placebo effect and they definitely found no evidence that such effects can be reliably reproduced. “To regard placebo acupuncture as a universally effective ‘super placebo’ would be inappropriate.” To get a ‘super placebo’ from acupuncture, you need rather a lot of emotional drama surrounding the treatment — which probably depends strongly on a perfect storm of psychological factors that just do not and cannot exist at a low-rent acupuncture office in a mini mall.43
There is a world of psychological difference between experiencing acupuncture in its native cultural context, and experiencing it as a commercialized fad in North America. I was in an acupuncturist’s office this morning, by chance. It had the usual cheesy alternative medicine decor — obligatory fountain, Chinese characters, Vitruvian Man on the business card, cheap diploma — and the acupuncturist was a shy young woman who couldn’t make eye contact, doubtless anxious to sell her services in a struggling economy. It was pretty uninspiring, honestly. In that bland environment, there was no chance of me getting swept up in a powerful placebo effect there … even if I wasn’t a skeptic.
Bonus acupuncture myth: no, acupuncture cannot induce labour in pregnant women
Legend has it that acupuncture can induce labour. This is widely believed and repeated uncritically by many sources. Unfortunately for our hopes and dreams, actual studies of this question have detected no clear sign of such a spooky power. It remains as elusive as psychic abilities.
A 2017 Cochrane Review tested the validity of the popular belief that stimulating specific acupuncture points can induce labour in pregnant women.45 Smith et al. analyzed the pooled results of 22 randomized controlled trials including over 3400 women. They looked for effects on labour induction and “cervical ripening” (softening prior to labour), mostly using acupuncture and acupressure. “Many” of the studies they included had at least some risk of bias, and therefore more likely to bend the data in favour of the belief… which didn’t really happen.
At most, there was weak evidence that acupuncture improves cervical ripening, which is an extremely weak-sauce result, like saying that you’ve captured Bigfoot and then showing off a chimpanzee wearing big rubber feet. Like a lot of meta-analysis these days, there’s almost always some slightly promising signal that the authors can cherry-pick (while invariably emphasizing the paucity and poor quality of evidence). But “a promising treatment is the larval stage of a disappointing one.”46
In every other way, “there were no clear differences” between any experimental groups for any other outcome, and there was “no clear benefit from acupuncture or acupressure.” If labour induction by acupuncture works at all, it’s obviously an unreliable and minor effect. The whole acupuncture-induces-labour thing is just another alternative medicine myth.
Acupuncture’s glory days are over
It’s all but over for acupuncture as a pain treatment. The science doesn’t just cast doubt on acupuncture — it puts more nails in the coffin, nails that are no longer necessary. In 2009, Madsen et al. wrote:
Our finding of limited, at best, analgesic effects of acupuncture corresponds with the seven Cochrane reviews47 on acupuncture for various types of pain, which all concluded that no clear evidence existed of an analgesic effect of acupuncture.
Madsen et al. was just confirming what was already painfully clear: the evidence was already overwhelming that there is simply nothing of great interest going on in acupuncture except some interesting placebo.
There’s always more to study, more to learn — but all of this evidence is certainly the death of any realistic hope that acupuncture is anything more than an ancient Chinese superstition. Even the most optimistic assessment of the existing scientific research can grant acupuncture no more than the slight possibility of subtle efficacy.
Whoop-de-doo. Who wants “subtle” when you’re in agony? Treating serious pain is serious business. There’s not much room for “subtle” benefits when you’re trying to help people who are in great pain.48
So it’s time to move on.
Acupuncture has seemingly been studied to death … and yet it will not die. It has a zombie like ability to live again as credulous reporters and health professionals write about the benefits after reading a poorly controlled study. Acupuncture produces a strong placebo effect and that’s it, and when studied with proper controls this has been verified again and again. Why won’t it just die already?
Melany Hamill, for Skeptic North
More studies are not the answer. No matter how many studies showed negative results, they would not persuade true believers to give up their beliefs. There will always be “one more study” to try, but there should be a common-sense point at which researchers can agree to stop and divert research time and funds to areas more likely to produce useful results.
Dr. Harriet Hall, Acupuncture Revisited
Fiddling while Rome burns
Acupuncture wouldn’t bother me so much if there were nothing better to think about, no better research to be discussing. But people are suffering from real, horrible chronic pain — they write to me every day, and statistics about chronic pain are thoroughly alarming — and there is urgent work to be done finding solutions for them, and educating both patients and professionals about realistic, rational options.
At best, acupuncture is a waste of valuable time — and now so is the debate about it. I haven’t heard an original or valid argument in defense of acupuncture in years,49 and I haven’t seen any compelling evidence ever , because it doesn’t exist. As every critic of acupuncture has explained ad infinitum, the most favourable evidence available is also the oldest, weakest and the most biased, and even that evidence is underwhelming, benefits that barely register as clinically significant — much ado about not much, even if it’s actually real, which no better study has ever confirmed.
Carl Sagan famously asked the Dalai Lama what would happen to Tibetan Buddhism if proof that there is no reincarnation could be found. The Dalai Lama sensibly replied:
Then Tibetan Buddhism would have to change.50
And it should be no different for acupuncture. If new evidence emerges that shows that it isn’t what we all hoped it would be, then it must change. That evidence has emerged. Practically everything I once optimistically believed/hoped about acupuncture has been crumbling for years. Science blogger Orac explains a similar evolution in his thinking about acupuncture:
Believe it or not, there was one area of so-called “alternative” medicine that I used to be a lot less skeptical about than I am now. Homeopathy, I always realized to be a load of pseudoscientific magical thinking. Ditto reiki, therapeutic touch, and other forms of “energy healing.” It didn’t take an extensive review of the literature to figure that out, although I did ultimately end up doing fairly extensive literature reviews anyway. Then, the more I looked into the hodgepodge of “healing” modalities whose basis is not science but rather prescientific and often mystical thought, the less impressed I was.
Even so, there was always one modality that I gave a bit of a pass to. There was one modality that, or so I thought, might actually have something to it. There was one modality that seemed to have a bit of suggestive evidence that it might do something more than a placebo. I’m referring to acupuncture. No, I never bought all the mystical mumbo-jumbo about how sticking needles into “meridians” somehow alters or “unblocks” the flow of a mysterious “life force” known as qi that is undetectable by science. I did wonder if perhaps it worked as a counterirritant or by releasing endorphins.
Then I actually started paying attention to the scientific literature regarding acupuncture, including literature like this and this. The more I read, the more I realized something. I realized that there was far less to acupuncture than I had previously thought, and, even with my previous openness to it, I hadn’t thought all that much about it anyway. What I had thought about it was that it might have a very mild beneficial effect. What I know now is that acupuncture is almost certainly no more than an elaborate placebo. What I know now is that virtually every study of acupuncture claiming to show a positive effect has serious methodological flaws and that the better-designed the study the less likely there is to be an effect.
Is acupuncture FDA approved?
No — only acupuncture needles themselves are approved as a Class II medical device (since 1996), not the practice of acupuncture itself. The FDA just requires needles to be sterile, non-toxic, labelled as single-use, and “used appropriately by licensed practitioners.”
In other words, they want acupuncture needles to be sharp, clean, and used with legitimate medical intent by trained people — as opposed to dull, dirty, and inserted under your fingernails by baristas. It’s a low bar.
Naturally, acupuncture practitioners often claim (or strongly imply) that FDA approval means that acupuncture works, that it is “endorsed” as effective (like here or here). This is ignorant and deceptive.
The FDA only requires evidence of efficacy for drugs (not proof). For everything else they regulate, they are focused on safety and function.51 In the case of acupuncture needles, FDA approval as “safe and effective” means that the needles will, in fact, safely puncture the skin when used appropriately — not that doing so is therapeutic.
And the FDA screws up, and their approval is hardly a guarantee of anything in any case. Just because they have certified something as safe and effective doesn’t mean it actually is. There’s a long history of embarrassing examples of things the FDA should never have approved!
Certainly FDA approval of acupuncture needles does not guarantee the safety of acupuncture…
Acupuncture safety: mostly safe, but not entirely
To conclude, and to add injury to insult, I want to emphasize that acupuncture is not just ineffective, but not even entirely safe.
Acupuncture needles may be FDA approved as safe when used as intended by licensed practitioners… but the words “as intended” are doing a lot of heavy lifting there, and licensing doesn’t guarantee competence, wisdom, or even common sense. Obviously acupuncture education isn’t exactly known for its devotion to science and physiology. Most acupuncturists sincerely believe we have magic energy fields, after all! They are on the record (in droves) claiming that acupuncture can treat COVID.
As with any treatment that breaks the skin, disastrous infection is possible, and outbreaks of mycobacteria infection caused by acupuncture have been reported in the last decade.52 Furthermore, placebo effects tend to backfire: the patient is betrayed in the end, and the failure to achieve a lasting cure paradoxically cements the patient’s idea their pain is untreatable, “even by acupuncture.”53
Ernst et al. did a good job of backing this up, and explained that “serious adverse effects continue to be reported,” such as infections and collapsed lungs. Nothing like a little sepsis and collapsed lung to add to the fun of chronic pain! Although assumed to be rare, some concerned Danish physicians who saw two cases in three months wonder if it “may not be so uncommon.”54
Of course these risks are not common complications. And when medicine works, costs and risks are acceptable, even a “no brainer.” But if there are no clear, consistent, measurable benefits to a treatment? Then there is no justification for any risk.
“Even if it could help in decreasing chronic pain, acupuncture still remains a passive intervention which doesn’t enhance confidence, self-efficacy & self-management of chronic pain.”
Did you find this article useful? Interesting? Maybe notice how there’s not much content like this on the internet? That’s because it’s crazy hard to make it pay. Please support (very) independent science journalism with a donation. See the donation page for more information & options.
About Paul Ingraham

I am a science writer in Vancouver, Canada. I was a Registered Massage Therapist for a decade and the assistant editor of ScienceBasedMedicine.org for several years. I’ve had many injuries as a runner and ultimate player, and I’ve been a chronic pain patient myself since 2015. Full bio. See you on Facebook or Twitter., or subscribe:
Appendix
A personal perspective: How it felt to change to my mind about acupuncture over a period of several years
I used to “believe” in acupuncture. I think almost everyone did. Probably not this guy. And probably not this one either. But just about everyone else, even skeptics, cut acupuncture some slack.
Over the years, I have been persuaded by more and more good quality evidence — and the steady stream of patients with nothing better to say about it than “maybe it helped for a while” — that there is really nothing at all to acupuncture. It’s just another folk medicine tradition, about as therapeutically meaningful as a manicure.
So how did it feel to change my mind? Oh, a little awkward. It was like diving into water you just know is cold enough to make you gasp. I felt some emotional resistance to the evidence. I also remember feeling comforted whenever I read anything that seemed to bolster my besieged beliefs , and there was plenty of that. It took me quite a while to notice the disturbing pattern that the evidence supporting acupuncture was of consistently lower quality, while the evidence undermining it was of consistently higher quality.
Things started to get more comfortable when I noticed that I rather liked the doctors, scientists and skeptics who were challenging acupuncture. They seemed ridiculously bright — and I like bright people. I actively seek out people who are smarter than I am, because I figure it’s the most obvious way to get smarter: you are who you hang out with. I certainly didn’t like them because they agreed with me on much of anything, because we didn’t agree at that time. But they won me over.
Having my beliefs challenged by such intelligent people was uncomfortable at first, but it was overshadowed by the desire to understand. Despite my initial reluctance, in the end I’m proud to say that I was much more interested in just knowing how the world works than anything else.
Related Reading
- Do You Believe in Qi? — How to embrace a central concept of Eastern mysticism without being a flake
- T’ai Chi Helps Fibromyalgia, but It’s Not “Alternative” Medicine — Despite a high profile boost from the New England Journal of Medicine, it’s still just gentle, elegant, and pleasant exercise
- “Science-Based Medicine Acupuncture Resource Page,” a collection of resources at ScienceBasedMedicine.org. SBM’s excellent resource pages examine a topic in detail from the perspective of science-based medicine, as opposed to evidence-based medicine.
- Acupuncture Anesthesia: A proclamation from Chairman Mao, an extraordinary series of articles explaining that acupuncture anaesthesia does not actually exist.
- Alternative Medicine’s Choice — What should alternative medicine be the alternative to? The alternative to cold and impersonal medicine? Or the alternative to science and reason?
- “Acupuncture research – the path least scientific?,” Neil O’Connell and G Lorimer Moseley, TheConversation.com. An excellent skeptical analysis of acupuncture from a couple of particularly credible authors and researchers. >There’s no doubt that acupuncture is gaining traction on the grounds that it holds up under scientific interrogation. But does it really? …Ensuring robust double-blinding studies of acupuncture is a tricky business. Nonetheless, good quality trials across a range of clinical conditions and outcomes, overwhelmingly show that acupuncture fails to outperform sham.
What’s new in this article?
Eleven updates have been logged for this article since publication (2009). All PainScience.com updates are logged to show a long term commitment to quality, accuracy, and currency. more
When’s the last time you read a blog post and found a list of many changes made to that page since publication? Like good footnotes, this sets PainScience.com apart from other health websites and blogs. Although footnotes are more useful, the update logs are important. They are “fine print,” but more meaningful than most of the comments that most Internet pages waste pixels on.
I log any change to articles that might be of interest to a keen reader. Complete update logging of all noteworthy improvements to all articles started in 2016. Prior to that, I only logged major updates for the most popular and controversial articles.
See the What’s New? page for updates to all recent site updates.
2022 — Added new section, “Is acupuncture FDA approved?”
2021 — Science update: acknowledged the drafted change in acupuncture recommendations from the UK’s influential guidelines from the National Institute for Health Care Excellence (NICE).
2021 — New section, “Bonus acupuncture myth: no, acupuncture cannot induce labour in pregnant women.”
2018 — New section, “A fine example of acupuncture research that seems well-designed and positive … but is still bizarrely flawed.”
2018 — Covered the fresh PLoS ONE scandal over “one of the worst acupuncture studies I have ever seen.”
2018 — Added two citations to the introduction to keep things fresh, and a good quote to the conclusion.
2018 — Added citation to Stenger et al. on pneumothorax risk.
2017 — Added citation to Vickers et al., with skeptical analysis.
2016 — Science updated — added citation to the NICE guidelines for low back pain.
2016 — Added a mobile-only article summary.
2016 — Significant science update. New short section about Chae et al., the “phantom acupuncture” study. Also added a couple related reading links, and a sidebar about spellings/meanings of “qi.”
2009 — Publication.
Notes
- Madsen MV, Gotzsche PC, Hrobjartsson A. Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups. BMJ. 2009;338:a3115.
The reviews concludes that “a small analgesic effect of acupuncture was found, which seems to lack clinical relevance and cannot be clearly distinguished from bias. Whether needling at acupuncture points, or at any site, reduces pain independently of the psychological impact of the treatment ritual is unclear.” In the context of treating pain, a “small analgesic effect” is nearly worthless, and it hopelessly damns with faint praise, and that’s assuming it’s even a genuine effect of acupuncture. In fact, it’s vastly more likely to be an effect of being handled and taken care of (“the treatment ritual”).
- Ernst E, Lee MS, Choi TY. Acupuncture: Does it alleviate pain and are there serious risks? A review of reviews. Pain. 2011 Apr;152(4):755–64. PubMed 21440191 ❐
A dozen of the best scientific studies of acupuncture treatments for pain were carefully analyzed in this review. The acupuncture treatments were for conditions like osteoarthritis, headache and migraine, low back pain, fibromyalgia, and more. The authors found a statistically significant but “small difference between acupuncture and placebo acupuncture.” They concluded that “the apparent analgesic effect of acupuncture seems to be below a clinically relevant pain improvement.” They also note that “serious adverse effects continue to be reported.”
Pain invited a well-known voice of reason in medicine, Dr. Harriet Hall, to write an editorial about this paper. Dr. Hall’s editorial is an easy-reading summary for both patients and professionals. It is reproduced in full on ScienceBasedMedicine.org: see Acupuncture Revisited.
- Ee C, Xue C, Chondros P, et al. Acupuncture for Menopausal Hot Flashes: A Randomized Trial. Ann Intern Med. 2016 Jan. PubMed 26784863 ❐
Real acupuncture once again fails to beat sham acupuncture, this time for menopausal hot flashes. Large trial, good methodology, fine journal, low risk of researcher bias … and completely consistent with the trend in acupuncture research: the better the test, the harder it fails.
Treatment of hot flashes is a classic claim made for acupuncture. - NICE.org.uk [Internet]. National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management; 2016 Nov [cited 23 Apr 13]. PainSci Bibliography 53641 ❐
- The 2020 draft of the NICE advice rather notoriously reversed its “do not offer” recommendation to a recommendation to “consider” it. The recommendation is based on “very low quality evidence from 13 studies” and “low quality evidence from 2 studies” … which is ridiculous. Garbage in, garbage out! If NICE changes its recommendations, it obviously won’t actually be based on good evidence — by their own admission. See: “UK Recommendations Wrong on Acupuncture: NICE draft recommendations on acupuncture don’t even make sense from an EBM perspective, and utterly fail to consider SBM principles.”)
- This is an annoying general trend in alternative medicine: exaggerating “the power of placebo” as a way to justify therapy that can’t beat it. Therapies that perform no better than placebo are now often spun as being “as good as placebo,” as though placebo is the new gold standard to meet. Acupuncture is the most glaring example of this, but the same trick has been pulled with homeopathy, chiropractic, scammy supplement products, and more. The phenomenon is described in full in Placebo Power Hype: The placebo effect is fascinating, but its “power” isn’t all it’s cracked up to be.
- An acupuncturist once confessed to me that he was considering retiring because the evidence so strongly shows that acupuncture is useless. After much hand-wringing conversation by email, in which he appeared to be on the brink of being super ethical and changing his career, he decided instead to keep his day job selling the power of placebo.
- Berman BM, Langevin HH, Witt CM, Dubner R. Acupuncture for Chronic Low Back Pain. N Engl J Med. 2010 Jul 29;(363):454–461. PubMed 20818865 ❐ PainSci Bibliography 54942 ❐
A bizarre and already infamous paper: bizarre because the authors clearly acknowledge that acupuncture is no better than a placebo, and bizarre because they conclude that it should be recommended, and most bizarre of all because it is published in The New England Journal of Medicine. Truly, one of the lowest moments in the history of that famous journal!
The best criticisms of the NEJM’s editorial choices here can both be found on Science-Based Medicine, by Drs. Crislip (NEJM and Acupuncture: Even the best can publish nonsense) and Novella (Acupuncture Pseudoscience in the New England Journal of Medicine). Dr. Crislip’s post is really quite funny.
- Cherkin DC, Sherman KJ, Avins AL, et al. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009 May;169(9):858–66. PubMed 19433697 ❐ PainSci Bibliography 54907 ❐
More than 600 participants were either given standard acupuncture treatments or simulated acupuncture. Although this study has been widely reported as if it was a controlled comparison of acupuncture to “standard medical treatment” for back pain, in fact it is not controlled (or blinded), and does not have the power to prove that acupuncture works for back pain.
The apparent difference between real and fake acupuncture they observed was minor. Nevertheless, the authors are excessively friendly to acupuncture and declare it to be “effective” in their conclusion in spite the obvious poverty of the data. In particular, they gloss over the damning implications of their most important finding: what little effect they think they found had nothing at all to do with needle placement. Acupuncture means nothing if needle placement doesn’t matter. The interpretation of Dr. Steven Novella is much more sensible: “The only reasonable scientific conclusion to draw from this is that acupuncture does not work.” For Dr. Novella’s meticulous and expert analysis, see Acupuncture Does Not Work for Back Pain (Part I).
- Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for Chronic Pain: Individual Patient Data Meta-analysis. Arch Intern Med. 2012 Sep:1–10. PubMed 22965186 ❐
The conclusion of this acupuncture meta-analysis sure sounds positive, but it’s the usual hard-spun, garbage-in-garbage-out, damned-with-faint-praise-anyway nonsense. The conclusion indicates that “acupuncture is more than a placebo” but the differences are too minimal to care, or to attribute to anything more than a sloppy, biased meta-analysis.
An editorial for the Huffington Post confidently, absurdly declares of this study, “It turns out acupuncture works. It's not a placebo, and it's not a scam. It's a technique with documented efficacy,” but the author’s next statement is “I have little to say about the evidence involved.” Clearly! What do actual experts say? Dr. Edzard Ernst: “In my view, this meta-analysis is the most compelling evidence yet to demonstrate the ineffectiveness of acupuncture for chronic pain.” Dr. Steven Novella:
The Vickers acupuncture meta-analysis, despite the authors’ claims, does not reveal anything new about the acupuncture literature, and does not provide support for use of acupuncture as a legitimate medical intervention. The comparison between true acupuncture and sham acupuncture shows only a small difference, which is likely not clinically significant or perceptible. More importantly, this small difference is well within the degree of bias and noise that [is] inherent in clinical trials.
- Vickers AJ, Vertosick EA, Lewith G, et al. Acupuncture for Chronic Pain: Update of an Individual Patient Data Meta-Analysis. J Pain. 2017 Dec. PubMed 29198932 ❐
I’ve been asked a lot about “the Vickers update” (this 2017 update to the original infamous paper, Vickers 2012).
Vickers clearly couldn’t come to a negative conclusion about acupuncture if his life depended on it. He’s about as biased as a researcher can get, and this more recent paper adds nothing of interest to what he’s published previously. Everything Dr. Steve Novella wrote about the 2012 meta-analysis is still completely relevant: “the so-called positive effects from meta-analyses such as Vickers are so razor thin that they are clinically insignificant (meaning explainable by even subtle bias or methodological flaws).” Vickers noticed the criticism, but his only rebuttal was to complain that skeptics are evil and dishonest.
- Cummings M, Hróbjartsson A, Ernst E. Should doctors recommend acupuncture for pain? BMJ. 2018 Mar;360:k970. PubMed 29514785 ❐ I know who I think won this debate, but of course it won’t convince anyone who believes in acupuncture. Although Ernst and Cummings make excellent arguments, I’m citing it as an example of the BMJ’s shit-disturbing for attention. The quote there is not from Dr. Ernst, but from Dr. David Colquhoun, another exceptionally qualified critic of pseudoscience, who acerbically tweeted about this paper. I completely agree: the BMJ is just perpetuating what is now much closer to a manufactroversy than a legit controversy, and they are probably doing it just for the sensationalism — tabloid tactics from a major scientific journal aren’t as unusual as you might think! This was a publication stunt as silly as a climate science journal publishing a debate with a climate change denier.
- Zhu L, Ma Y, Deng X. Comparison of acupuncture and other drugs for chronic constipation: A network meta-analysis. PLoS One. 2018;13(4):e0196128. PubMed 29694378 ❐ PainSci Bibliography 53227 ❐ Really, it’s just incredibly bad: “a new wrinkle in bad acupuncture meta-analyses”; “nonsense on a whole other level, shame on @PLOSONE” ; so bad that it provoked Dr. Steven Salzberg to resign from their editorial board.
- American Academy of Orthopaedic Surgeons. Treatment of Osteoarthritis of the Knee – 2nd Edition. AAOS.org. 2013. PainSci Bibliography 54555 ❐ Along with glucosamine, chondroitin, “lube jobs” (injection of joint lubricant), and surgical lavage and debridement. What does work? Exercise, weight loss, and painkillers are praised.
- Chicago Tribune [Internet]. Tsouderos T. CAM: Taxpayer money spent on studies with questionable scientific value; 2011 Dec 16 [cited 12 Feb 19].
NCCIH has also gotten around no-better-than-placebo findings essentially by fluffing up the importance of the placebo effect and claiming that it is inherently interesting. Tsouderos explains: “To most scientists, that would mean the treatments are failures — drug companies cannot sell medicines that work no better than salt water or a sugar pill. But in the case of acupuncture and other mind and body medicine, the center and its supporters say it’s unclear whether the benefits represent a placebo response or something more complicated” — something more complicated meaning, basically, a really good placebo effect.
Officially, and with regards to other kinds of treatments like saw palmetto, “NCCIH considers studies finding that a supplement does no better than a placebo to be evidence that it does not work.” But NCCIH has failed to apply the same standard to acupuncture, and continues to spend vast sums of money to prove over and over again that acupuncture cannot do better than placebos.
“And yet, instead of declaring these studies convincingly negative, NCCIH is pouring more research money into acupuncture. ‘The intellectual dishonesty is just astounding,’ said Dr. Steven Novella, a neurologist at Yale School of Medicine and a critic of NCCIH. ‘They are just quietly changing the question and the rules.’
- Rosa L, Rosa E, Sarner L, Barrett S. A close look at therapeutic touch. JAMA. 1998 Apr 1;279(13):1005–10. PubMed 9533499 ❐ PainSci Bibliography 56856 ❐
This paper is an entertaining chapter in the history of the science of alternative medicine: a child’s science fair project published in the Journal of the American Medical Association. Emily Rosa’s experiment showed that “twenty-one experienced therapeutic touch practitioners were unable to detect the investigator's ‘energy field.’ Their failure to substantiate TT's most fundamental claim is unrefuted evidence that the claims of TT are groundless and that further professional use is unjustified.”
Therapeutic touch practitioners could not demonstrate any ability to detect a person by feeling their aura, let alone manipulating it therapeutically. The test made them look ridiculous.
Ms. Rosa was just nine years old when she did this experiment, and remains the youngest person to have a research paper published in a peer reviewed medical journal. (It is, of course, likely that she had some parental assistance — but I don’t know the whole story.)
- Historically, skeptics often acknowledged that traditional Chinese medicine is so extremely different from medicine as we know it in Europe and North America that there was probably something of medical interest going on, somewhere, somehow, in the world of acupuncture. It’s easy to state the case so broadly that it’s nearly impossible to disagree with: yes, there’s probably “something” of medical interest, “somewhere” in traditional Chinese medicine! As evidence accumulated, however, skeptics have turned against acupuncture en masse.
- Li Y, Zheng H, Witt CM, et al. Acupuncture for migraine prophylaxis: a randomized controlled trial. Canadian Medical Association Journal. 2012 Mar;184(4):401–10. PubMed 22231691 ❐ PainSci Bibliography 54425 ❐
This is a disturbing and typical example of sloppy modern acupuncture research, methologically flawed in several ways with clearly negative results, despite the fact that it was clearly built to give acupuncture an unfair advantage, by researchers who wanted to prove that acupuncture works. They concluded that acupuncture has only “a clinically minor effect on migraine,” damning with (very) faint praise, but even that is a biased exaggeration — cherry-picking the best results, and ignoring the more important negative ones. As summarized by Dr. Steven Novella for ScienceBasedMedicine.org: “Despite all of these shortcomings, all of which would bias the study in the direction of being positive, the study was negative. For the primary outcome measure there was no statistically significant difference between any of the acupuncture groups and the sham acupuncture group.”
- Vickers A, Goyal N, Harland R, Rees R. Do certain countries produce only positive results? A systematic review of controlled trials. Control Clin Trials. 1998 Apr;19(2):159–66. PubMed 9551280 ❐
Apparently “research conducted in certain countries was uniformly favorable to acupuncture.” Russia and China in particular effectively do not publish any negative results about acupuncture. I love this ripe, juicy understatement: “Publication bias is a possible explanation.” YA THINK?!
- Green S, Buchbinder R, Hetrick S. Acupuncture for shoulder pain. Coch. 2005;(2):CD005319. PubMed 15846753 ❐ PainSci Bibliography 54322 ❐ This 2005 review of acupuncture for shoulder pain is one of the most popular of all Cochrane reviews, but it’s a disappointing review of only a handful of mostly crappy little studies (9) that clearly states that “there is little evidence to support or refute the use of acupuncture for shoulder pain,” but the authors bend over backwards anyway to acknowledge that “there may be short-term benefit with respect to pain and function.” This is based on scraps of incredibly unimpressive and unreliable data: “The improvements with acupuncture for pain and function were about the same as the effects of receiving a fake therapy for 2 to 4 weeks.” Emphasis mine.
- Manheimer E, White A, Berman B, Forys K, Ernst E. Meta-analysis: acupuncture for low back pain. Ann Intern Med. 2005;142(8):651–663. PubMed 15838072 ❐
- Schultz IZ, Crook J, Meloche GR, Berkowitz J, et al. Psychosocial factors predictive of occupational low back disability: towards development of a return-to-work model. Pain. 2004 Jan:77–85. PubMed 14715392 ❐
This study identified factors affecting return-to-work time after an episode of low-back pain. From the abstract: “The key psychosocial predictors identified were expectations of recovery and perception of health change.”
- Molsberger AF, Schneider T, Gotthardt H, Drabik A. German Randomized Acupuncture Trial for chronic shoulder pain (GRASP) - a pragmatic, controlled, patient-blinded, multi-centre trial in an outpatient care environment. Pain. 2010 Oct;151(1):146–54. PubMed 20655660 ❐
- BodyInMind.org [Internet]. O’Connell N. Location location location! Acupuncture and chronic shoulder pain: CAM or Sham?; 2011 Mar 8 [cited 18 Jun 13]. PainSci Bibliography 55223 ❐
- O’Connell N, Wand B, Goldacre B. Interpretive bias in acupuncture research? A case study. Eval Health Prof. 2009 Dec;32(4):393–409. PubMed 19942631 ❐
This is a discussion of an article about the use of acupuncture for chronic low-back pain. “The authors suggest that interpretive bias has affected reporting, leading to questionable conclusions and advocacy in favor of this form of care that may exceed the evidence. They also suggest that a lack of understanding of research into the placebo effect may have contributed to confusion in the interpretation of these trials.”
For a good related example, see author Neil O’Connell’s criticism of Molsberger et al., a paper that shows a “positive” result from acupuncture but has an absurdly glaring flaw.
- Fake acupuncture involves the insertion of needles into non-acupuncture points, or the use of non-penetrating needles (kind of like a stage dagger, where the blade collapses into the handle). It may be difficult or impossible for the patient to tell whether or not they are receiving “real” acupuncture. “For example,” Madsen et al. write, “when patients are asked whether they feel qi, a high proportion of patients will say yes, even when they have been treated with a non-penetrating placebo acupuncture needle.” Bizarre and a bit funny, patients will even “feel the chi” when the needles are — I’m not making this up — being stuck in a rubber hand. More on this below, but you can definitely fool people into feeling, and the sensations are associated with what the brain thinks is going on, and not what is actually happening in tissue.
- Many proponents of acupuncture have griped about this, arguing that the fake is not an effective control. They are missing the forest for the trees. It’s true, it’s certainly not a perfect control — but it’s good enough (and a heck of a lot better than no control at all). If acupuncture worked, it should be dramatically superior to any fake. Trying to argue your way out of that takes mental gymnastics.
- Vas J, Aranda JM, Modesto M, et al. Acupuncture in patients with acute low back pain: A multicentre randomised controlled clinical trial. Pain. 2012 Sep;153(9):1883–9. PubMed 22770838 ❐
- Madsen et al.’s analysis shows that real acupuncture works slightly better than placebo — but by so little that it’s not even remotely exciting. The difference could easily just be due to the fact that real acupuncture is somehow a little bit more convincing, on average, than sham acupuncture — and thus there’s a slightly strong placebo effect.
- Chae Y, Lee IS, Jung WM, et al. Psychophysical and neurophysiological responses to acupuncture stimulation to incorporated rubber hand. Neurosci Lett. 2015 Feb;591C:48–52. PubMed 25681621 ❐
- This is a well-established technique, a kind of optical illusion achieved with mirrors. It’s a very cool effect: you can cause pain by banging a rubber hand with a hammer. See Rubber hand illusion
![]() 2:15.
2:15. - ScienceBasedMedicine.org [Internet]. Kavoussi B. The Acupuncture and Fasciae Fallacy; 2011 Jan 13 [cited 14 Sep 24]. PainSci Bibliography 54882 ❐
In this article, Ben Kavoussi explains that acupuncture its current form is a modern invention of the pediatrician Cheng Dan’an (承淡安, 1899-1957) in the early 1930s.
- Ramey D, Buell PD. A true history of acupuncture. Focus on Alternative and Complementary Therapies. 2004;9(4):269––273. PainSci Bibliography 53782 ❐
- ScienceBasedMedicine.org [Internet]. Ramey D. Acupuncture and history: The “ancient” therapy that’s been around for several decades; 2010 Oct 18 [cited 20 Sep 10]. PainSci Bibliography 54827 ❐
It seems that just about every article about acupuncture makes some reference to it having been used in China for thousands of years. The obvious reason for such a statement is to make the implication that since it’s been around for so long, it must therefore also be effective. Of course, longevity doesn’t argue for efficacy, otherwise everyone would likely agree that astrology is the way to chart one’s life; astrology has been practiced for many more years than acupuncture. What’s maddening about the acupuncture longevity myth is that it isn’t true, and demonstrably so.
Some readers have complained that there were indeed needles and meridians and points in ancient Chinese medicine, and therefore it is ancient. There were recognizeable antecedents to the modern forms of “points” and “meridians” and “needling.” However, they were so different that there is no meaningful continuity between them. David Ramey elaborated on this for me via email:
There is nothing from the time that describes what was actually done. When we have descriptions and pictures, it shows something wildly different from modern acupuncture. And, yes, the ancient Chinese used “needles.” The first written description of the needles was that of ten Rhijne, which showed that the needles were large awls that were pounded in with a hammer. I have a Japanese picture from the early 1600s that showed that the “needles” were lancets and hooks (not needles). And, yes, there were channels (“mai”). The points didn’t necessarily rest on the channels, and there were all sorts of different channel maps. But all this eventually turned into today’s mostly French interpretation (Soulie de Morant).
Ergo, modern acupuncture is its own thing, and ancient acupuncture-ish practices were clearly something else.
- ScienceBasedMedicine.org [Internet]. Hall H. The Reality of Ancient Wisdom: Acupuncture and TCM Weren’t So Great; 2014 Sep 25 [cited 15 Mar 29]. PainSci Bibliography 53776 ❐
- Quah SR. Traditional healing systems and the ethos of science. Social Science & Medicine (1982). 2003 Nov;57(10):1997–2012. PubMed 14499521 ❐
Stella Quah on how traditional Chinese medicine is failing to adapt to modern times:
… the pressure to comply with official health regulations and the inability to succeed under the ethos of science lead traditional Chinese medicine practitioners to respond with an ethos of pragmatic healing that eschews conceptual analysis, ignores the paradigmatic divide with biomedicine, and focuses on ‘using what works’.
So it’s a nasty mess.
- ScienceBasedMedicine.org [Internet]. McKenzie B. How popular is acupuncture?; 2011 Mar 28 [cited 12 Feb 19]. PainSci Bibliography 55276 ❐
- Kanodia AK, Legedza ATR, Davis RB, Eisenberg DM, Phillips RS. Perceived benefit of Complementary and Alternative Medicine (CAM) for back pain: a national survey. J Am Board Fam Med. 2010 May-Jun;23(3):354–62. PubMed 20453181 ❐ PainSci Bibliography 54984 ❐
Alternative medicine for back pain is not as popular as most people assume. I was surprised myself when a 2010 American survey found that only about 6% of the US population uses any kind of alternative therapy for their back pain: about 75% chiropractic, 20% massage therapy, a few percent acupuncture, and a few percent divided up between everything else. Still, 6% of the American population is almost 2 million people annual looking for a crack, rub, or needle poke!
- Although unsubstantiated and extremely difficult to prove, there seems to be evidence that several kinds of chronic pain, especially low back pain, have become much more common than they used to be. See The Complete Guide to Low Back Pain for some more information about that.
- More about what I hear from patients and readers: I understand and appreciate that “cured” patients would probably not have come to see me later on for the same problem. However, I’m really plugged into the lives of a lot of pain patients, and there is simply no theme of acupuncture-cure stories. No one comes in for wrist pain and comments that “I used to have neck pain, too, but it was cured by an acupuncturist.” The stories just aren’t there, in my experience. The stories that are there are the failure stories. Seemingly every other patient who’s been through the “therapy grinder” (tried everything) has received acupuncture that did little or nothing to help them.
- ScienceBasedMedicine.org [Internet]. Atwood KC. Acupuncture Anesthesia: A proclamation from Chairman Mao; 2009 May 15 [cited 12 Feb 19]. PainSci Bibliography 55489 ❐
- The wishful thinker will be inclined to say, “But maybe there is an effect and it’s just erratic, hard for science to pin down!” Perhaps. But any effect that is so hard for science to pin down that we can’t even prove it exists is also next to useless in practice. If a standardized treatment protocol can’t deliver the goods in a somewhat reliably fashion, it’s not really medicine — or at least it’s not medicine I want to spend my money on until its “erratic” nature is better understood. See also Most Pain Treatments Damned With Faint Praise.
Practitioners of alternative medicine often imply that they have “great power” by talking up their “great responsibility” to avoid the dangerous side-effects of their allegedly potent methods. It’s a self-serving way to inflate the perception of potency while seeming adult and professional about it! It’s also an easy position to defend, because it makes critics seem reckless — you have to be quite sure of your facts to warn anyone to ignore a safety warning! With the Great-Power Gambit, “everyone wins” except the truth.
Unsurprisingly, the actual harms of alternative medicine tend to get ignored, while mainly the more fanciful ones are exploited for this purpose.
- Smith CA, Armour M, Dahlen HG. Acupuncture or acupressure for induction of labour. Cochrane Database Syst Rev. 2017 10;10:CD002962. PubMed 29036756 ❐ PainSci Bibliography 51735 ❐
- Bastian H. "They would say that, wouldn't they?" A reader's guide to author and sponsor biases in clinical research. J R Soc Med. 2006 Dec;99(12):611–4. PubMed 17139062 ❐ PainSci Bibliography 51373 ❐
The full quote:
“A promising treatment is often in fact merely the larval stage of a disappointing one. At least a third of influential trials suggesting benefit may either ultimately be contradicted or turn out to have exaggerated effectiveness.”
- Cochrane reviews are generally considered to be the most authoritative summaries of the science on a topic so far.
- Paula Kamen writes brilliantly (and hilariously) about the inadequacy of “subtle” treatments in All in My Head: An epic quest to cure an unrelenting, totally unreasonable, and only slightly enlightening headache.
- When I published my own reaction to Ernst et al., many critics voiced their opinion at me on Facebook, with great contempt. They were angry, but they couldn’t actually defend their position. They could not and did not actually produce any evidence, and they (angrily) repeated myths that have long since been debunked, like the myth that acupuncture is used for anesthesia in China. I cannot emphasize strongly enough that this is what it’s always like: the apologists come out of the woodwork to shout and pound the table, but they never have persuasive data, sound logic or consistent reasoning, or even basic historical accuracy on their side.
- Of course, he also made it clear that he didn’t think it was bloody likely that anyone could ever prove that negative, and of course he’s right about that. It’s also rather hard to prove that there’s no teapot orbiting the sun between the Earth and Mars. But his initial answer certainly had the right spirit — evidence matters. If it can be had.
- For instance, FDA approval of food additives and medical devices mainly just means “probably safe.” For medical devices, which includes everything from lasers to acupuncture needles, they officially require “valid scientific evidence that there is a reasonable assurance that the devices are safe and effective for their intended uses” (FD&C Act Chapter V: Drugs and Devices, section §360d, “Performance standards”). What they mean by “effective” is not medically beneficial (“efficacious”), but just that it does what it says on the tin. For example, FDA approval of a laser therapy device means that it does in fact emit lasers •pew pew!• and it won’t hurt people when used appropriately… not that doing so is known to solve any medical problem.
- Woo PCY, Lin AWC, Lau SKP, Yuen KY. Acupuncture transmitted infections. BMJ. 2010 Mar 18;340:c1268Oh, I. PubMed 20299695 ❐ PainSci Bibliography 55627 ❐
What’s the harm in acupuncture? A small but real risk of infection — as with anything that breaks the skin. Acupuncture has not only failed to prove that it works, but this British Medical Journal editorial presents new evidence that it also involves a risk of mycobacteria infection, and even that “ … outbreaks of acupuncture transmitted infections may be the tip of the iceberg. The first reports of meticillin resistant S aureus (MRSA) transmitted by acupuncture appeared in 2009. The emergence of community associated MRSA infections may aggravate the problem.”
A common objection to Woo’s article has been that it is “mongers fear” and that he cites old evidence, from the 1970s and 1980s, before sterilized needles were widely used. But critics conveniently overlook that Woo also cite modern evidence of infection — about as blatant a case of biased interpretation as you could ask for. And is Woo a fear mongerer? He does not claim that the risk is great: he just reports what is known and titles his piece neutrally. It is always worthwhile to examine treatment risks, and especially when treatment benefits are also hotly disputed. It hardly constitutes “fear-mongering” to report risk data in a medical journal! If not there, then where?
- Working as a Registered Massage Therapist, I routinely saw placebo backfire in this way. Pain patients in general, and low back pain patients in particular, are already strongly predisposed to anxious assumptions that their problem is “really bad.” When the placebo effect of acupuncture wears off, as it must, this anxiety is reinforced and the pain is elevated to the status of a fiercer enemy. A nice trap. I describe this in a little more detail in The Complete Guide to Low Back Pain
- Stenger M, Bauer NE, Licht PB. Is pneumothorax after acupuncture so uncommon? J Thorac Dis. 2013 Aug;5(4):E144–6. PubMed 23991325 ❐ PainSci Bibliography 52811 ❐
ABSTRACT
Acupuncture is one of the most widely used forms of traditional Chinese medicine often referred to as alternative therapy in the Western World and over the past decades it has become increasingly popular in Denmark. Pneumothorax is known as the most common serious complication following acupuncture, but it is quite rarely reported. During a three-month period two patients with pneumothorax caused by acupuncture were admitted to our department. The purpose of this case report is to increase awareness of this complication, which may not be so uncommon.

